Medical Services
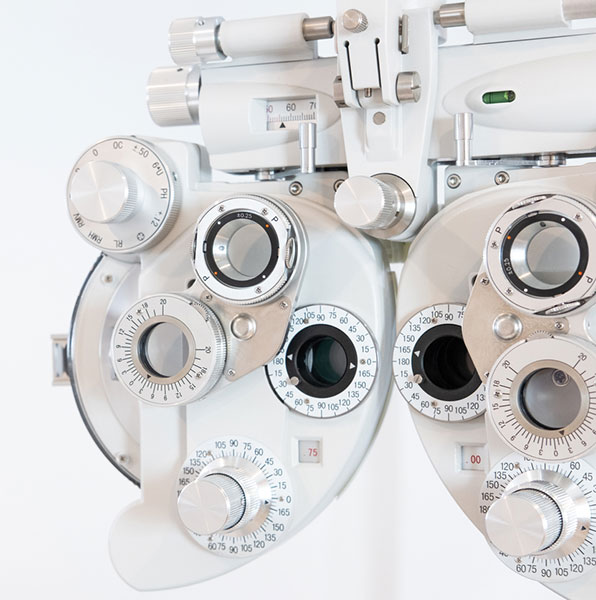
Comprehensive Eye Exams
Regular eye exams for the entire family are important in maintaining your eyes’ health by detecting and preventing disease. Some diseases may develop slowly without causing pain or vision loss. Early detection of problems can reduce the risk of further harm and allow for a choice of treatment options. Using state-of-the-art equipment and expert diagnostic skills, we regularly screen for diseases such as glaucoma, diabetic retinopathy and macular degeneration, which can develop without any noticeable symptoms.
Patients should see their eye doctor for a comprehensive eye exam every one to three years, depending on their age, risk of disease and overall physical condition. Children should have regular eye examinations to ensure the proper development of their vision and prevent any interference with their academic achievements. Older adults are often at a higher risk for eye conditions such as macular degeneration, glaucoma, and cataracts. Even though your eyes seem healthy, you should still have regular eye examinations to detect any problems as soon as possible and begin necessary treatment.

Corneal Exams
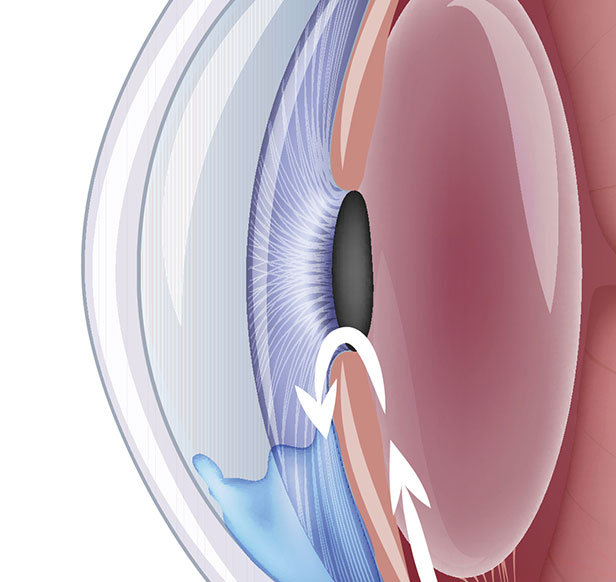
The cornea is the clear covering of the front of the eye that bends, or refracts, light rays as they enter the eye. For clear vision to occur, the cornea must have the correct shape and clarity to focus incoming light rays precisely on the retina at the back of the eye.
Corneal exams are important because they can determine whether any distortions exist in this portion of the eye. A computerized test called corneal topography can map out the surface of the cornea, alerting your doctor to the presence of inflammation, scarring or astigmatism. This exam can provide information about the health of the cornea and is a valuable diagnostic tool prior to a contact lens fitting, vision correction procedure or corneal transplant.
Diabetic Eye Disease
Patients with diabetes are at a higher risk of developing eye conditions as a complication of their disease. These conditions can lead to vision loss and blindness and include diabetic retinopathy, cataracts and glaucoma. Diabetic retinopathy is actually the leading cause of blindness in the United States.
Diabetic eye conditions often develop without any noticeable loss of vision or pain, so significant damage may have occurred by the time patients notice any symptoms. For this reason, it is important for diabetic patients to have their eyes examined at least once a year. Early detection of eye disease can help prevent permanent damage.
Diabetic eye conditions can be detected through a comprehensive eye exam. A comprehensive eye exam involves a visual acuity test to measure vision at various distances, and a dilated eye exam to examine the structures of the eye for any signs of disease. During this test, your doctor can examine the retina and optic nerve with a special magnifying lens. Tonometry may also be performed during a comprehensive eye exam to measure the pressure inside the eye with a special instrument.
Other than controlling blood pressure, blood cholesterol and the levels of blood sugar, treatment is not needed during the first three stages of diabetic retinopathy. The fourth stage, proliferative retinopathy is treated with a laser surgery procedure known as scatter laser treatment. During the procedure the abnormal blood vessels are ablated causing them to shrink. This procedure works best once the blood vessels begin to bleed. Severe blood vessel bleeding may need to surgically corrected with a vitrectomy procedure to remove the blood from the eye.
Patients with diabetes need to have an annual comprehensive dilated eye exam. The length of time a patient has diabetes will determine the likelihood of developing diabetic retinopathy. Almost 50 percent of patients in the United States, diagnosed with diabetes, have a form of diabetic retinopathy.
The risks of developing diabetic eye disease can be minimized by:
- Monitoring changes in vision
- Keeping A1C levels under 7%
- Monitoring and managing blood pressure levels
- Eating a healthy diet
- Participating in a regular exercise routine
- Monitoring and managing cholesterol levels


Dry Eye Disease Management
Dry eye is a common condition that occurs when the eyes are insufficiently moisturized, leading to itching, redness and pain from dry spots on the surface of the eye. The eyes may become dry and irritated because the tear ducts don’t produce enough tears, or because of a chemical imbalance in the tears. Patients with dry eyes often experience irritating symptoms that may result in more serious damage to the vision if the condition is left untreated.
Treatment for dry eye depends on the cause and severity of the condition, as well as the patient’s overall health and personal preference. Non-surgical treatments are often effective, and may include increasing humidity levels at home or work, use of artificial tears or a moisturizing ointment and avoiding air conditioning or windy conditions outdoors.
Tears are normally produced by the lacrimal gland and flow across the eye, as we blink, and eventually flow into the punctii, 2 openings in the eyelids, near the nose. The tears subsequent flow into the nasolacrimal sac which empties into the nose. An effective way to treat dry eyes is to occlude the openings, the punctii, preventing tears from leaving the eyes. Occlusion can be achieved by inserting small silicone plugs into the openings, the punctii. This procedure can be performed safely and effectively in our office by Dr. Matthews.
Glaucoma
Glaucoma is a group of related diseases that damage the optic nerve, resulting in vision loss and possible blindness. Many people affected with glaucoma do not experience symptoms, and may not be aware that they have the disease until they have lost a significant amount of vision. With early detection and treatment, however, eyes can be protected against the serious loss of vision or blindness. Catching glaucoma at an early, treatable stage is one important reason to have regular, thorough eye examinations. A leading cause of blindness and visual impairment in the United States, glaucoma affects patients of all ages.
There are several factors, including the following, that increase the risk of developing glaucoma:
- Being older than 60
- Being of particular descent, such as African-American or Asian
- Having a family history of glaucoma
- Having elevated intraocular pressure
- Having poor vision, or other eye disorders or injuries
- Having certain medical conditions, such as diabetes
- Taking certain medications, such as corticosteroids, for prolonged periods
The diagnosis of glaucoma is made after a comprehensive medical examination of the eye, and a review of the patient's medical history. Tests are conducted to confirm the diagnosis. Testing may include the following:
- Tonometry
- Dilated-eye examination
- Visual field test (perimetry)
- Retinal evaluation
- Pachymetry
- Gonioscopy
- Visual acuity test
Once glaucoma is diagnosed, treatment should begin as soon as possible to help minimize the risk of permanent vision loss.
There is no cure for glaucoma, so treatments, including those below, focus on relieving symptoms and preventing further damage.
Medication
Eye drops or oral medication may be used to either reduce fluid production in the front of the eye or to help drain excess fluid. Medication requires regular use to keep eye pressure under control.
Laser Surgery
Trabeculoplasty, iridotomy and cyclophotocoagulation are laser procedures that aim to increase the outflow of fluid from the eye, or eliminate fluid blockages.
Other Surgery
A trabeculectomy creates a new channel to drain fluid from the eye, and reduce the pressure that causes glaucoma. Surgery is performed only after medication and laser procedures have been unsuccessful.

Thyroid Eye Disease Care
Hyperthyroidism, also known as an overactive thyroid gland, involves an excess of hormone production that can lead to weight loss, irregular heartbeat and irritability. One of the most common reasons for an overactive thyroid gland is Graves’ disease, an autoimmune disorder in which antibodies cause the thyroid to produce too much thyroxine.
Graves' disease is diagnosed through a physical examination and a blood test to determine the patient's serum level of thyroid hormones. Imaging tests such as a CT scan or MRI scan may also be performed. Since the thyroid gland requires iodine to produce its hormones, the physician may also order a radioactive iodine uptake test.
This condition may cause symptoms involving the eyes such as bulging, redness of the eyes, excess tearing, swollen eyelids and light sensitivity. If symptoms are mild, conservative treatment may be attempted using lubricating eye drops, protective eye coverings and prism lenses. Oral steroids are sometimes prescribed for short-term use to relieve swelling and discomfort.
In more severe cases of thyroid eye disease, surgical treatment may be recommended. Depending upon the way the condition is affecting the eyes, procedures may be considered to relieve the pressure on the optic nerve, reposition the muscles of the eye or alter the eyelid skin and tissue.